Focus areas
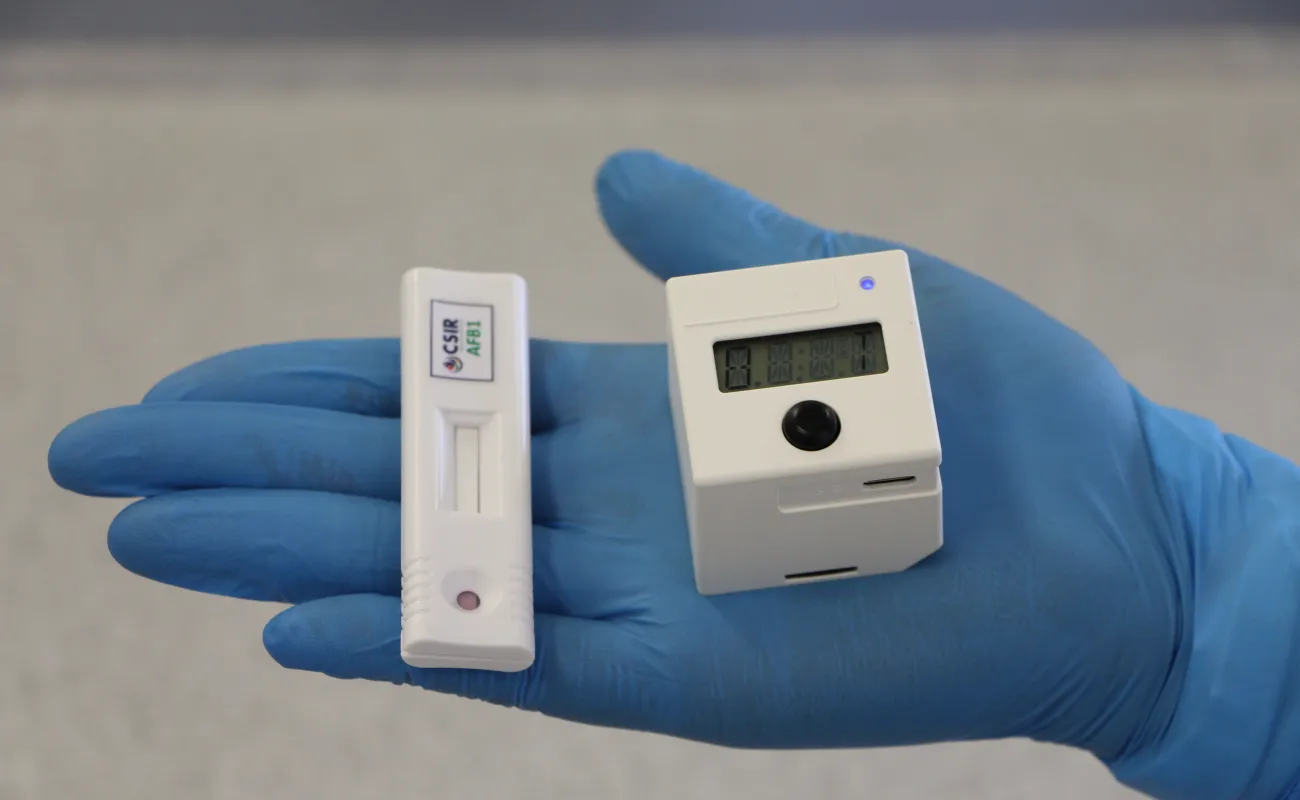
Diagnostics
We conduct pioneering research and development to create affordable diagnostic assays for point-of-care applications, ensuring pandemic preparedness. We expertly navigate the full development value chain, transforming concepts into validated prototypes to strengthen local diagnostic manufacturing capabilities.
View more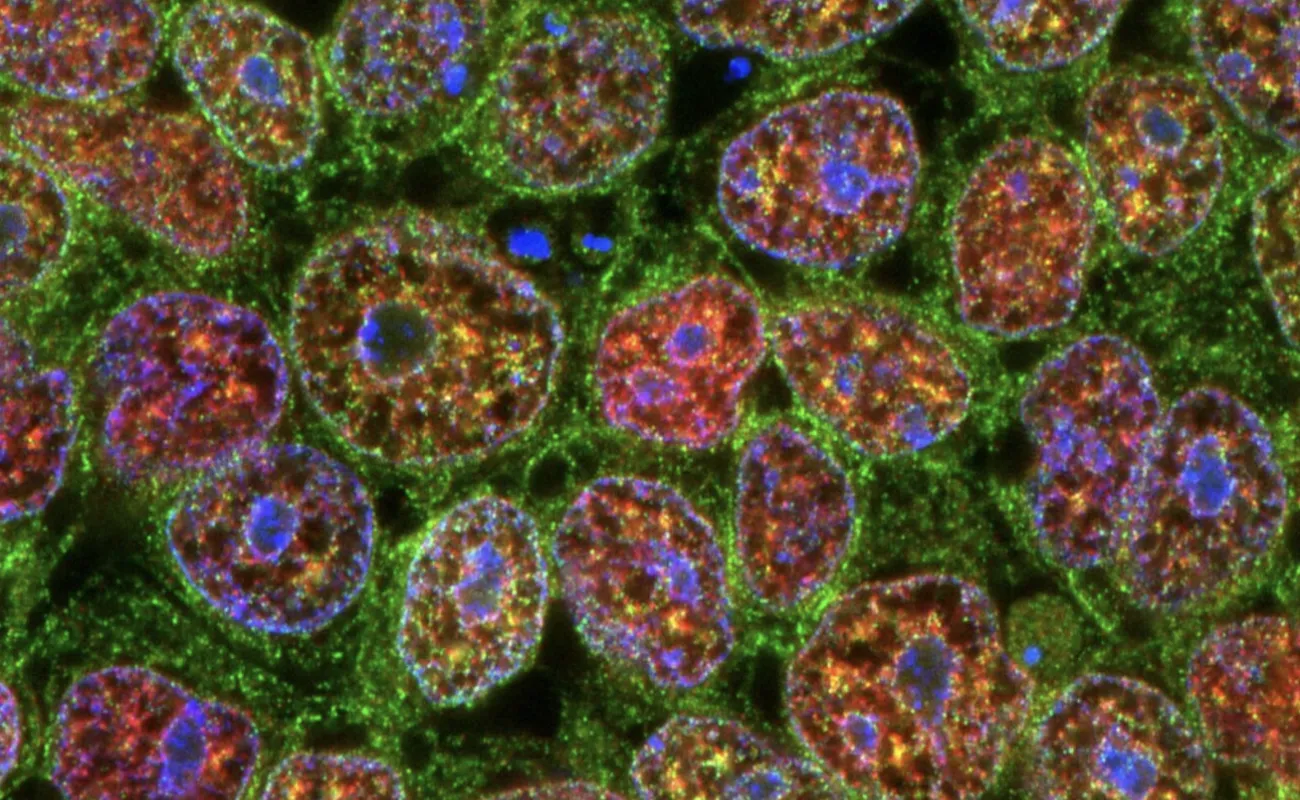
Genomics
We focus on embedding African genetics into the global drug development pipeline to improve treatment outcomes and reduce adverse drug reactions for African populations. By leveraging stem cells and genome engineering, we develop advanced preclinical tools. In addition, we explore the microbiome and other omics layers to develop digital precision medicine solutions tailored to African health profiles.
View more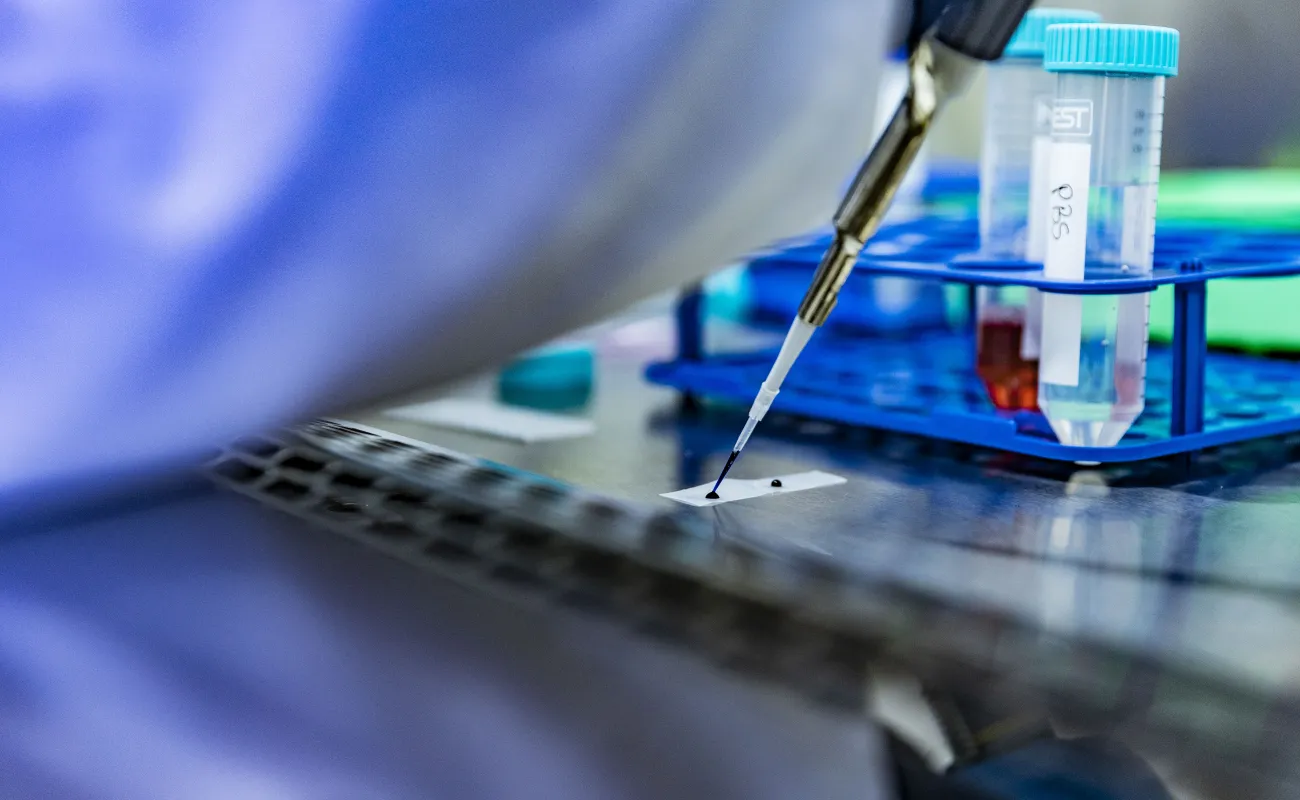
Precision oncology
We conduct cancer research with a focus on understanding the unique genetics and drug sensitivity that influence cancer treatment in African populations. Through inclusive science, innovation and data-driven health solutions, we aim to advance equitable and effective diagnostics and treatments. Using our novel drug sensitivity test, we are transforming access to cancer care in Africa and beyond.
View more
Synthetic biology
We develop synthetic biology capabilities by integrating engineering principles into bio-designs, developing new biological parts and redesigning existing biological systems to deliver solutions in agriculture, food, chemicals, biomanufacturing and health. Our work includes therapeutic applications such as cancer precision medicine, multi-omics, stem cell technology, synthetic microbial chassis and drug repurposing.
View more
Vaccines and biotherapeutics
We develop new vaccine candidates, biologics and diagnostic tools, including reagents for innovative rapid, on-site testing kits. From early-stage research to clinical-stage investigational products, we support regional health systems and aim to position South Africa as a self-sufficient developer and producer of these health products.
View more

